Ventilation Quick Guides
As part of the Project Firstline initiative, ASHE, in collaboration with the American Hospital Association (AHA), has released Ventilation Guidance and Quick Guides for health care workers, staff, and facility managers so that they can confidently make knowledgeable evidence-based decisions regarding ventilation in health care settings to keep patients and staff safe and reduce chance of contamination and infection from diseases that spread through the air. One guide is designed for health care facility managers and the other is for nurse managers and clinicians.
Nurse Manager and Clinicians Quick Guide
This Quick Guide is meant to be a reference with short answers for frequently asked questions regarding ventilation and infection control in the health care environment. Detailed information for all Quick Guide FAQs can be found in Infection Control Guidance on HVAC for Nurse Managers and Clinicians.
Download the Guidance for Nurse Managers and Clinicians SPANISH Version
-
What is the purpose of an HVAC system?
- Heating or cooling of spaces.
- Adjusting relative humidity of air.
- Establishing directional airflow or pressurization relationships between spaces.
- Filtering and diluting recirculated air.
- Flushing contaminants in the air from enclosed spaces.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Introduction” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
How can I develop an effective means of communication about an HVAC system with the facilities team?
- Develop a working knowledge of features and limitations of HVAC system.
- Understand which types of patients should be housed in certain rooms.
- Facilities team should inform clinical leaders when HVAC equipment is not operating or in need of repair.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Communication” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
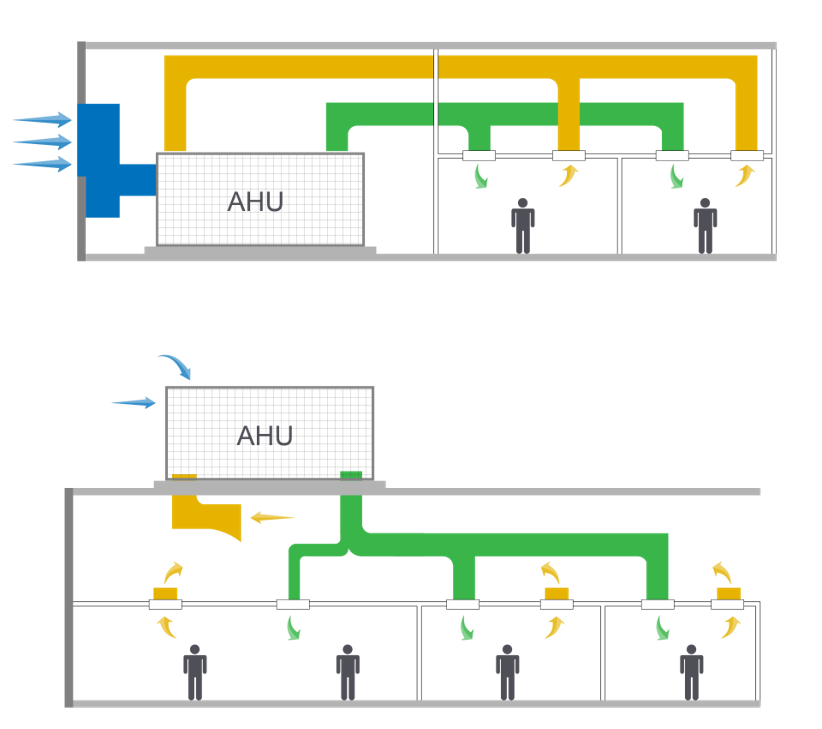
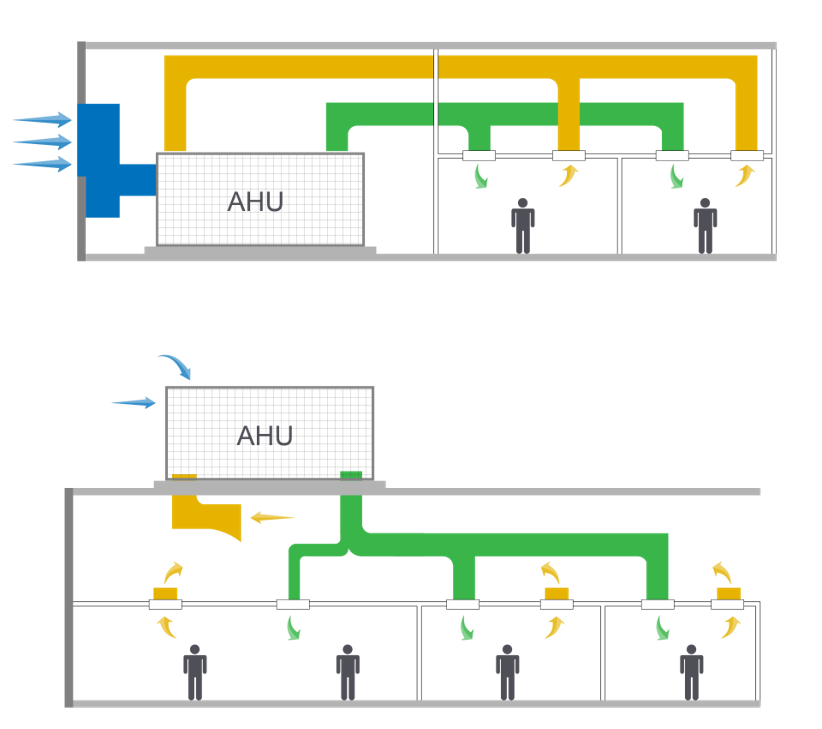
How is fresh OSA brought into a health care facility
- Fresh OSA is brought into the building by the HVAC system.
- The HVAC system will mix fresh OSA with return air (RA) recirculated from the building.
- The mixed air is cooled and/or heated, then filtered and supplied to the building.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Introduction” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What is an HVAC System's role in infection control?
- Continuous airflow through spaces to dilute contaminant levels (air change).
- Filtration of delivered air to remove contaminants.
- Exhausting air as appropriate to remove contaminants, preferably at their source.
- Using HVAC system air balance to create air pressure differentials when required from space to space.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Introduction” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What is positive or negative pressure?
- Pressurization in heating ventilating and air-conditioning (HVAC) refers to the relative pressure between spaces.
- A pressure relationship is established by providing more air than would be required into a space, and return or exhausting the excess air from an adjacent space.
- This directional airflow keep contaminants out of the positive room, and inside the negative room.
View from inside negative pressure room: Tissue paper shows air flowing into room.

View from inside positive pressure room: Tissue paper shows air being sucked from the room.

Setting reference: Inpatient and outpatient facilities.
For more information, see “Pressurization” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What is air filtration and what do I need to know about it?
- Filters work by capturing or absorbing airborne contaminants.
- Filters are rated on a Minimum Efficiency Reporting Value (MERV) scale.
- The higher the MERV rating the higher the dilution levels.
- A high efficiency particulate air (HEPA) filter is rated for at least 99.97% efficiency, which delivers air cleaner than the highest MERV (MERV 16) or fresh outside air.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Filtration” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What is MERV?
- Minimum Efficiency Reporting Value is a term defined in ASHRAE Standard 52.2 referring to the filters ability to capture airborne particles.
- Rating value developed by ASHRAE to report a filters ability to capture particles at varying size. A higher MERV rating indicates a higher performing filter.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Filtration” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What is AIIR and when should one be used?
- AIIRs are designed to hold individuals who have an airborne infectious disease.
- AIIRs have a higher airflow requirement, meaning more air is delivered to the space.
- An AIIR has a directional airflow or pressurization requirement to be under negative pressure from adjacent spaces.
- All of the air supplied to an AIIR is discharged or exhausted to the outside of the building.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Airborne Isolation Infection Rooms (AIIRs)” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What are the recommendations for facilities without an AIIR when a patient is infected with an airborne infectious disease?
- Put the individual in a treatment room, alone with the door closed and a medical mask.
- Wait until the individual is able to be safely moved to a more robust facility (i.e., an inpatient facility with AIIRs).
- Consult the table for the amount of time that must elapse before entering or using the room again.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Communication” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What is an anteroom, and what is its purpose?
- A small room between an airborne infection isolation room (AIIR) and an adjacent space.
- Creates a buffer for protection between the AIIR and adjacent space.
- An anteroom should be treated like an airlock, with doors always kept closed except when entering or exiting the anteroom.
- An anteroom should never be used for storage except as dictated by clinical staff for donning/doffing of personal protective equipment (PPE).
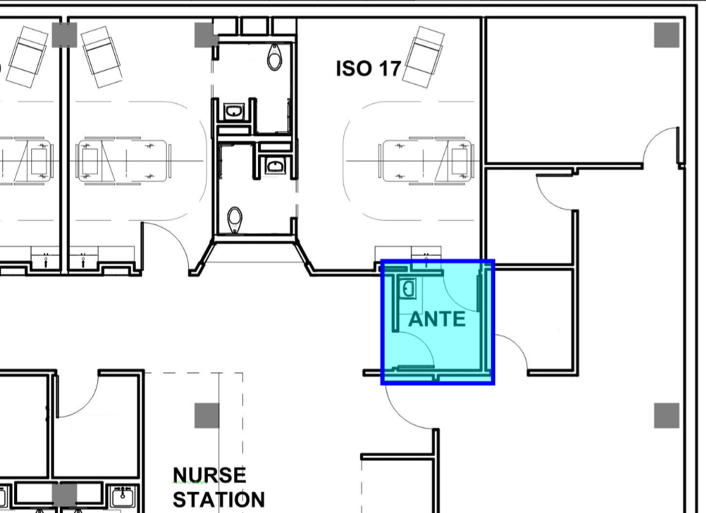
Setting reference: Inpatient and outpatient facilities.
For more information, see “Anteroom” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
how is an AIIR different from other types of patient rooms?
- AIIRs have a higher airflow requirement, meaning more air is delivered to the space.
- An AIIR has a directional airflow or pressurization requirement to be under negative pressure from adjacent spaces.
- All of the air supplied to an AIIR is discharged or exhausted to the outside of the building.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Airborne Isolation Infection Rooms (AIIRs)” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What is an ACH rate?
An ACH is the amount of times the volume of air in a room will be replaced in 1 hour.
ASHRAE 170 defines the minimum amount of ACH various spaces must have:
ACH=(60 x CFM)÷V
or
CFM=(ACH x V)÷60- CFM = cubic feet per minute [ft/min] (airflow rate)
- V = volume [ft] (room size)
- 60 = constant for number of minutes in an hour
Setting reference: Inpatient and outpatient facilities.
For more information, see “Dilution” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
Is increasing a room's ACH an effective measure to increase infection control practices?
- No.
- Increasing a room’s ACH rate can have unintended effects such as altering the pressurization between spaces.
- Rooms designed and operating to the requirements of ANSI/ASHRAE/ASHE Standard 170 have adequate airflow for health care activities taking place in those spaces.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Pressurization” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
How much time is required to elapse before using a room if an infectious individual was inside?
Consult the table below for the length of time for the 99% and 99.9% particle removal based on air change per hour (ACH) rate.
It is recommended to wait for the 99.9% efficiency duration.
ACH 99% Efficiency (minutes) 99.9% Efficiency (minutes) 2 138 207 4 69 104 6 46 69 7 35 52 10 28 41 12 23 35 15 18 28 20 14 21 50 6 8 Setting reference: Inpatient and outpatient facilities.
For more information, see “Dilution” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
Do some facilities have cleaner air than others?
- Yes.
- Licensed inpatient facilites have some of the cleanest air of all buildings.
- There is a wide range and gradient to the robustness and performance of HVAC systems.
- Outpatient and other facility types (e.g., medical office buildings or ambulatory surgery centers may not have the same provisions of a licensed inpatient facility).
Setting reference: Inpatient and outpatient facilities.
For more information, see “Introduction” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What should I do if I am concerned about the ventilation, temperature or humidity levels in a room?
- Confirm the thermostat is set to the correct temperature.
- Confirm the humidity sensor (if one is present and displays a reading) is within the acceptable range, generally 40%-60% relative humidity.
- If there are still concerns with the HVAC of a room, clinical staff leaders should understand which team members should communicate with the facilities team to address and correct any issue.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Relative Humidity” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
-
What is ceiling plenum?
- A ceiling plenum refers to the space above a ceiling and below the roof or floor above.
- Some heating ventilating and air-conditioning (HVAC) systems use this enclosed space as a pathway to return air to the HVAC equipment.
- This type of construction is not permitted for inpatient facilities due to the possibility of unintended particle migration from space to space.
Setting reference: Inpatient and outpatient facilities.
For more information, see “HVAC Equipment” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Nurse Managers and Clinicians.
Health Care Facilities Managers Quick Guide
This Quick Guide is meant to be a reference with short answers to frequently asked questions regarding ventilation and infection control in the health care environment for Facilities staff members. Detailed information for all Quick Guide FAQs can be found in Infection Control Guidance on HVAC for Facilities Managers.
Download the Guidance for Health Care Facilities Managers SPANISH Version
-
What is an HVAC system’s role in infection control?
- Continuous airflow through spaces to dilute contaminant levels (air change).
- Filtration of delivered air to remove contaminants.
- Exhausting air as appropriate to remove contaminants, preferably at their source.
- Using the HVAC system air balance to create air pressure differentials when required from space to space.
- Flushing contaminants in the air from enclosed spaces.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Introduction” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
How can I develop an effective means of communication with the clinical team about HVAC systems?
- Develop a working knowledge of functions and procedures of different departments.
- Understand which types of patients should be housed in certain rooms.
- Inform clinical leaders when HVAC equipment is not operating or in need of repair.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Communication” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
How is fresh OSA brought into a health care facility
- Fresh OSA is brought into the building by the HVAC system.
- The HVAC system will mix fresh OSA with return air (RA) recirculated from the building.
- The mixed air is cooled and/or heated, then filtered and supplied to the building.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Introduction” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is the best first step to take when considering HVAC system upgrades or renovations?
- Engage with reputable and experienced architects and engineers.
- Filtration of delivered air to remove contaminants.
- Always survey and perform a test and balance (TAB) prior to any upgrades.
- Note that any area renovated or upgraded must be brought up to the current code cycle.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Introduction” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
How often should ventilation systems be inspected?
- An HVAC ventilation system should be inspected at least once a year.
- System testing can be verified by using a supply air measuring hood (balometer).
- System testing and balance should be performed as required, as well as before and after any renovations.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Brief Resource Review” and "System Upgrades" in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is positive or negative pressure?
- Pressurization in (HVAC) refers to the relative pressure between spaces.
- A pressure relationship is established by providing more air than would be required into a space, and return or exhausting the excess air from an adjacent space.
- This directional airflow keep contaminants out of the positive room and inside the negative room.
View from inside negative pressure room: Tissue paper shows air flowing into room

View from inside positive pressure room: Tissue paper shows air being sucked from the room.

Setting reference: Inpatient and outpatient facilities.
For more information, see “Pressurization” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is air filtration and what do I need to know about it?
- Filters work by capturing or absorbing airborne contaminants.
- Filters are rated on a Minimum Efficiency Reporting Value (MERV) scale.
- The higher the MERV rating the higher the dilution levels.
- A high efficiency particulate air (HEPA) filter is rated for at least 99.97% efficiency, which delivers air cleaner than the highest MERV (MERV 16) or fresh outside air.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Filtration” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
Are ventilation and filtration upgrades required for an inpatient facility?
- Increasing filtration is a good strategy for air cleaning and to increase dilution.
- Fan power levels must be examined prior to increasing filtration levels to confirm there is enough power to operate as designed with upgraded filters.
- Licensed inpatient facilites already have high filtration levels of MERV 14 in health care areas.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Filtration” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is high efficiency particulate air (HEPA) filtration?
- High efficiency particulate air (filter).
- HEPA filters are high efficiency air filters designed to capture at least 99.97% of airborne contaminants.
- HEPA filters are capable of cleaning the air to a point that the air they discharge is even more clean than fresh outside air.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Filtration” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
When and where are portable high efficiency particulate air (HEPA) filtration units required?
- A portable HEPA filter’s primary purpose is to establish a pressurization relationship between two spaces.
- Portable HEPA filters also have the added bonus of filtering the air that is used to pressurizer a space.
- Potable HEPA filters can be used to establish a buffer zone or safe space between
Setting reference: Inpatient and outpatient facilities.
For more information, see “Filtration” and "Other Factors" in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is MERV?
- Minimum Efficiency Reporting Value is a term defined in ASHRAE Standard 52.2 referring to the filters ability to capture airborne particles.
- Rating value developed by ASHRAE to report a filters ability to capture particles at varying size. A higher MERV rating indicates a higher performing filter.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Filtration” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
MERV Rating Average particle size efficiency (PSE) 0.3-1.0 microns Average particle size efficiency (PSE) 1.0-3.0 microns Average particle size efficiency (PSE) 3.0-10.0 microns 1 < 20% 2 < 20% 3 < 20% 4 < 20% 5 20%-34.9% 6 35%-49.9% 7 50-69.9% 8 < 50% 70%-84.9% 9 < 50% ≥ 85% 10 50%-64.9% ≥ 85% 11 65%-79.9%% ≥ 85% 12 80%-89.9% ≥ 90% 13 < 70% ≥ 90% ≥ 90% 14 75%-84.9% ≥ 90% ≥ 90% 15 85%-94.9% ≥ 90% ≥ 90% 16 ≥ 95% ≥ 95% ≥ 95% HEPA ≥ 99.97% ≥ 99.97% ≥ 99.97%
-
What is AIIR and when should one be used?
- AIIRs are designed to hold individuals who have an airborne infectious disease.
- AIIRs have a higher airflow requirement, meaning more air is delivered to the space.
- An AIIR has a directional airflow or pressurization requirement to be under negative pressure from adjacent spaces.
- All of the air supplied to an AIIR is discharged or exhausted to the outside of the building.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Airborne Isolation Infection Rooms (AIIRs)” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is an anteroom, and what is its purpose?
- An anteroom is a small room between an AIIR and an adjacent space.
- Creates a buffer for protection between the AIIR and adjacent space.
- An anteroom should be treated like an airlock, with doors always kept closed except when entering or exiting the anteroom.
- An anteroom should never be used for storage except as dictated by clinical staff for donning/doffing of personal protective equipment (PPE).
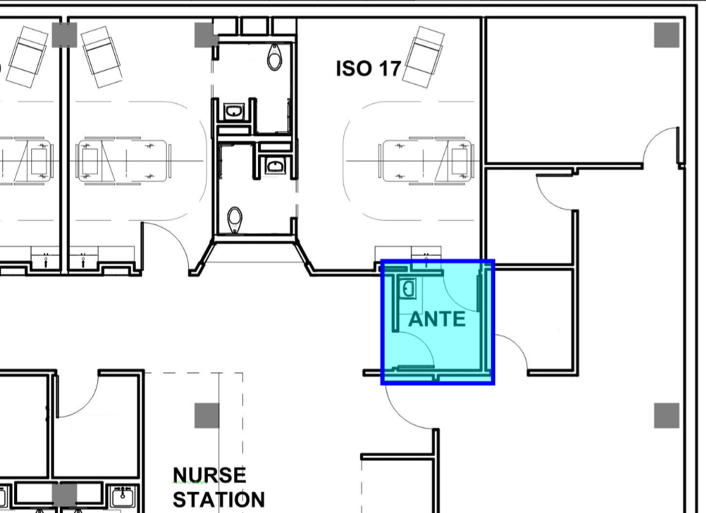
Setting reference: Inpatient and outpatient facilities.
For more information, see “Anteroom” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
How can I verify my airborne infection isolation room (AIIR) is functioning correctly?
- Verify the room pressure monitor is reading at least -0.01 inw.g.
- Keep a record of engineering drawings, test and balance report, and maintenance log to have a record for comparison.
- Verify AIIR is still within balancing numbers with a balometer.
- Have maintenance perform visual inspections of the equipment.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Airborne Infection Isolation Rooms (AIIRs)” and “Pressure Monitors” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is an ACH rate?
An ACH is the amount of times the volume of air in a room will be replaced in 1 hour.
ASHRAE 170 defines the minimum amount of ACH various spaces must have:
ACH=(60 x CFM)÷V
or
CFM=(ACH x V)÷60- CFM = cubic feet per minute [ft/min] (airflow rate)
- V = volume [ft] (room size)
- 60 = constant for number of minutes in an hour
Setting reference: Inpatient and outpatient facilities.
For more information, see “Dilution” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
How much time is required to elapse before using a room if an infectious individual was inside?
Consult the table below for the length of time for the 99% and 99.9% particle removal based on air change per hour (ACH) rate.
It is recommended to wait for the 99.9% efficiency duration.
ACH 99% Efficiency (minutes) 99.9% Efficiency (minutes) 2 138 207 4 69 104 6 46 69 7 35 52 10 28 41 12 23 35 15 18 28 20 14 21 50 6 8 Setting reference: Inpatient and outpatient facilities.
For more information, see “Dilution” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is the American Society of Heating, Refrigeration and Air-Conditioning Engineers (ASHRAE)?
- A society of engineers dedicated to providing HVAC standards for buildings.
- Three of the most important standards from an infection control perspective are:
- ASHRAE Standard 52.2, Method of Testing General Ventilation Air-Cleaning Devices for Removal Efficiency by Particle Size
- ASHRAE 62.1, Ventilation for Acceptable Indoor Air Quality
- ANSI/ ASHRAE/ASHE Standard 170, Ventilation of Health Care Facilities
Setting reference: Inpatient and outpatient facilities.
For more information, see “Brief Review of Resources” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
Do some facilities have cleaner air than others?
- Yes.
- Licensed inpatient facilites have some of the cleanest air of all buildings.
- There is a wide range and gradient to the robustness and performance of HVAC systems.
- Outpatient and other facility types (e.g., medical office buildings or ambulatory surgery centers may not have the same provisions of a licensed inpatient facility).
Setting reference: Inpatient and outpatient facilities.
For more information, see “Other Factors” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What should I do when extraordinary conditions arise such as those during a pandemic event?
- Rely on the basics of ventilation such as continuous airflow, exhausting dirty or contaminated areas, and establishing pressure relationships.
- Understand that pressure relationships are carefully engineered and field balanced as such.
- Increasing supply air to or exhaust air from a space may seem like a good idea, but can have unintended outcomes if not examined holistically.
Setting reference: Inpatient and outpatient facilities.
For more information, see “Introduction” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.
-
What is ceiling plenum?
- A ceiling plenum refers to the space above a ceiling and below the roof or floor above.
- Some heating ventilating and air-conditioning (HVAC) systems use this enclosed space as a pathway to return air to the HVAC equipment.
- This type of construction is not permitted for inpatient facilities due to the possibility of unintended particle migration from space to space.
Setting reference: Inpatient and outpatient facilities.
For more information, see “HVAC Equipment” in the Infection Control Guide on Heating, Ventilation and Air Conditioning for Health Care Facilities Managers.


