Focus on Compliance EC.02.02.01 | ASHE
FOCUS on EC.02.02.01
EC.02.02.01 – THE HOSPITAL MANAGES RISKS RELATED TO HAZARDOUS MATERIALS AND WASTE
RESOURCES FOR FACILITY PROFESSIONALS
ISSUE
Hospitals use hazardous materials and chemicals for a variety of day-to-day operations. These materials and chemicals come in many forms, from radioactive materials needed to perform diagnostic testing to medications prescribed and the cleaners used to sterilize patient treatment areas. Many of these materials pose potential health hazards such as irritation, sensitization, and carcinogenicity, as well as potential physical hazards such as flammability, corrosion, and radiation exposure. Management of hazardous materials and waste is required to ensure that these risks are properly managed and to ensure that information about the hazards and associated protective measures is disseminated to those who use or are exposed to materials.
RISK
Health care workers face a number of safety and health hazards. They include bloodborne pathogens and biological hazards; potential chemical and drug exposures; waste anesthetic gas exposures; respiratory hazards; ergonomic hazards from lifting and repetitive tasks; laser hazards; workplace violence; hazards associated with laboratories; and radioactive material and x-ray hazards. Some of the potential chemical exposures include formaldehyde, used for preservation of specimens for pathology; ethylene oxide, glutaraldehyde, and paracetic acid used for sterilization; and numerous other chemicals used in health care laboratories. The Occupational Safety and Health Administration (OSHA) has created a website outlining various hazards faced by health care workers.
IMPACT
Hazardous material and waste management is primarily focused on keeping those who work with these hazardous materials safe. Injuries can impact health care organizations in many ways, including lost worker productivity, increased costs, and possible fines or penalties. As institutions devoted to healing, hospitals should place a high priority on the proper protection of their employees to keep them safe and healthy.
MITIGATION
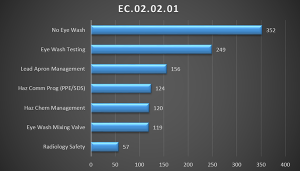
A review of 2014 Joint Commission survey data indicates the following key areas of noncompliance to Standard EC.02.02.01:
EYE WASHES ARE NOT AVAILABLE OR ARE NOT PROPERLY ACCESSIBLE, AND ARE NOT PROPERLY INSTALLED, TESTED, AND INSPECTED
OSHA requirements for emergency eyewashes and showers, found at 29 CFR 1910.151(c), specify that "where the eyes or body of any person may be exposed to injurious corrosive materials, suitable facilities for quick drenching or flushing of the eyes and body shall be provided within the work area for immediate emergency use."
ANSI/ISEA Z358.1 Standard for Emergency Eyewashes and Shower Equipment sets the guidelines for safety equipment fixtures and installation practices. While this is a voluntary standard, OSHA and accrediting organizations often use it as a guide when surveying facilities. In general, Z358.1 requires that emergency equipment be installed within 10 seconds walking time from the location of a hazard (approximately 55 feet) and the path from the hazard to the equipment should be free of obstructions and as straight as possible. The standard also requires that tepid water be provided to hard plumbed devices and defines this as water between the temperatures of 60 ͦ - 100 ͦ F (16 ͦ - 38 ͦ C).
Also, Z358.1 requires that a weekly activation test be performed to confirm proper operation of eye washes. The standard requires that maintenance be performed on these devices per the manufacturer’s operation and maintenance instructions. Many manufacturers provide specific check lists and tags for these inspections, which can be used to properly document the tests and inspections.
- 29 CFR 1910.151(c)
- OSHA Safety and Health Topics – Eye and Face Protection
- OSHA Eye and Face Protection eTool
PROTECTIVE LEAD APRONS OR COVERS ARE NOT PROPERLY STORED TO AVOID DAMAGE
Health care employees who work with radiographic equipment can be exposed to radiation, which can cause somatic (body) and/or genetic (offspring) injuries. The degree of exposure depends on the amount of radiation, the duration of exposure, the distance from the source, and the type of shielding in place. Exposure occurs when unprotected employees are near a machine in operation. The OSHA ionizing radiation standards found in 29 CFR 1910.1096 require that all individuals working in or frequenting any portion of a radiation area shall be instructed in the applicable provisions of this section for the protection of employees from exposure to radiation or radioactive materials. Radiation protection garments—lead aprons, protective collars, gloves, etc.—are worn by health care workers to reduce the effects of the radiation doses to which they are exposed during radiography procedures. These garments offer protection for workers and patients and should be worn in the direct x-ray field. These garments are required to be individually inventoried, annually tested for integrity, and handled and stored to avoid damage. Improper storage can cause cracks and holes in the protective lead lining allowing undue exposure to radiation.
Resources:
- 29 CFR 1910.1096 – Ionizing Radiation Standard
- OSHA Clinical Services Radiology – Radiation Exposure
- OSHA Technical Manual – Hospital Investigations: Health Hazards Section VI: Chapter 1
STAFF USING CHEMICALS DO NOT USE PROPER PERSONAL PROTECTIVE EQUIPMENT (PPE) OR MANAGE HAZARDOUS MATERIALS
Management of hazardous materials and waste is required to ensure that risks are properly managed and that information about the hazards and protective measures is disseminated to those who use or are exposed to materials. OSHA’s Hazard Communication Standard is designed to reduce risks and properly communicate hazards and protective measures to workers who use hazardous materials and chemicals. As of June 1, 2016, hospitals must be compliant with the OSHA Hazard Communication Standard 2012, as outlined in the Inside ASHE article listed in the resources below.
Resources:
- OSHA Hazard Communication
- OSHA Safety and Health Topics – Healthcare
- OSHA - What is Hazard Communication?
- Inside ASHE Article – Staying in Compliance with OSHA’s Hazard Communication Standard
ANALYSIS OF THE 2014 JOINT COMMISSION FINDINGS FOR EC.02.02.01
ASHE analyzed 2014 Joint Commission findings of EC.02.02.01 and found the following breakdown of the 1,177 findings documenting failure to manage risks related to hazardous materials and waste.