COVID-19 Recovery
Introduction
The COVID-19 pandemic is impacting the health care physical environment in ways we never imagined. Facilities have been reimagined, renovated, expanded, enlarged and underutilized simultaneously. The pandemic’s significant impact on the physical environment has offered challenges and learning experiences. Our reaction to this emergency has required agile assessments, multiple mitigations, perpetual preparation and rapid responses, and it will require a resolute recovery.
Up to this point, most emergency responses have been based on a local response, as most disasters are local events (e.g., local surge, hurricane, earthquake, fire or blizzard). Some disasters impact significantly large geographical areas, but until now none have impacted the entire nation and the world at large. The large-scale response to this pandemic has invited a broader scope of perspective to emergency management. While surge response specifically is focused on local health care coalitions, the procuring and distribution of personal protective equipment (PPE) is happening on facility, coalition, state, regional and federal levels. This multilevel approach has created confusion and frustration for many involved and especially for those in need of PPE.
Recovering from the impacts of this pandemic and documenting lessons learned are vital and will require significant planning and action. Not only will it require facilities to reimagine their responsibilities to their service population, but it will also require them to coordinate reopening with their coalition and state. This guide has been developed to assist health care facility managers in planning for and carrying out recovery measures to restore operational capabilities to appropriate post-COVID-19 pandemic levels.
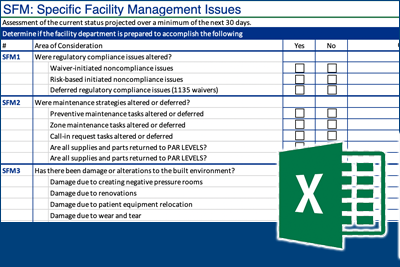
Specific Facility Management Issues
Since this guide is focused on recovering the health care physical environment, it is important to begin with the specific issues unique to the physical environment. There are many other recovery aspects that will need to be addressed in conjunction with those listed in this guide, but ASHE strongly encourages identifying individuals to focus on recovering these specific issues to prevent potential and significant harm.
Altered Regulatory Compliance Issues. Facilities managers should assess what regulatory compliance issues were altered during the response phase. With the declaration of a national emergency, the Centers for Medicare & Medicaid Services (CMS) was allowed by the Social Security Act Section 1135 to issue blanket waivers to provide flexibilities to assure access to health care. During this pandemic CMS issued multiple blanket waivers. Additionally, some states and local jurisdictions issued waivers to their specific regulatory compliance issues. A thorough assessment of these waivers will be required to ascertain that any regulatory compliance issues that were altered or deferred during the event are properly accounted for.
Altered Maintenance Strategies. Facilities managers should evaluate any alterations or deferments made to maintenance strategies during efforts to assist with significant patient surges. Assessing these changes and determining the necessary workload to rectify the subsequent backlog is critical. Without this evaluation, a significant amount of workload exclusive to facility management will be overlooked and could have a detrimental impact to the overall recovery efforts.
Damage to Built Environment. Damage to the built environment and the workload required to make repairs will also need evaluation. Consider damage from the creation of negative pressure rooms, the relocation of patient care equipment outside of the patient rooms, and wear and tear on the facility due to the surge, as well as damage to ductwork or HVAC changes/modifications.
Sustainability Measures. Determine the pandemic’s impact on sustainability measures implemented within the organization. Areas that might have been impacted include: energy management systems that may have been overridden, set back or turned off to meet surge demands on the facility or other modifications due to the surge such as schedules or ventilation measures that have been modified, water or waste conservation measures that have been modified and any changes within the fleet management strategy for the organization.
Necessary Workload. As mentioned in the paragraphs above, consider the overall workload necessary to get spaces back to normal operations. This will most likely be a gradual process that will require a dedicated effort from many different departments. Specific facility management issues to consider include: deferred maintenance issues, accessibility/restrictions to facility entrances, new signage, alternate care sites that were temporarily established, and if environmental assessments need to be performed in underutilized/closed areas before restoring to normal use.
Once a workload evaluation is completed, develop a staffing response plan for the determined workload. This staffing recovery effort should acknowledge any impacts to facility staff during the event, such as furloughs, reassignments, hiring freezes, etc. In addition, consider if any assessment of staff conditions is needed due to the pandemic. Having a thorough understanding of the current staffing situation will be imperative when developing the staffing response plan.
The development of a detailed staffing plan to address the predicted workload during the recovery phase is crucial to presenting a comprehensive recovery plan to administration, including the resources needed to accomplish the plan. This plan will help establish clear expectations regarding optimizing the physical environment in recovery from the pandemic.
Administrative Issues. Finally, during recovery, facilities managers should not forget to address key administrative issues such as capturing valuable data from a lessons learned event with the facility staff, updating the emergency plan and recognizing staff for the vital services they provided during the response efforts.
Pre-recovery Planning
Creating a successful pre-recovery plan is similar to reverse engineering an incident command event, and requires key aspects of all the operations involved. All key parties need to work together to develop and execute strategies and changes after considering the recovery from multiple perspectives. Some key topics to consider as your organization recovers from the pandemic are listed below. Keep in mind that the details and priority of these topics may differ based upon your organization’s location, size and scope of services.
- Global and Local Forecasts
- Currently, state and local officials are developing guidelines to help the country return to normal. It is critical that those guidelines are reviewed and considered in the development of your pre-recovery plan. This may include changes in services at the state and/or local level. The Centers for Medicare & Medicaid Services (CMS) has changed some reimbursements and restrictions related to providing care to patients. Tracking those changes will be important in plan development, particularly regarding other “reduction in capacity” stress and how to restart deferred services. Travel restrictions may need to be included depending upon locations and services.
- Participating in modeling forecasting for the organization with transition from organization’s current volumes to projections of various volumes moving forward including admissions, surgeries, emergency department visits, clinic visits, etc. to provide planning for workload and staffing. This process will help with the facility review to assure that changes like social distancing and visitor protocols will continue to function as clinical volumes increase. Examples of some challenges include: Are waiting areas big enough to handle volumes? How will food service and other amenities be delivered in this transition?
- Working with planning and strategy office/department or operations section to help determine workload impacts. Schedule when various facility resources will need to be brought online or transitioned to a new care delivery methodology. Consider your accommodations for asymptomatic patients and staff, and screening and treatment areas for confirmed COVID patients. Are organizations going to cohort and separate these patients to help reduce risk? If this is the case, how will various services be delivered to these patients in your organization?
- Financial
- Review budget projections from impacts of reduction in services. Can spaces be closed to reduce expenses if needed? Can building systems operations be changed to reduce energy costs?
- Gather and document costs and losses. Work with finance department and set up either early in the process or leave for post-opening. Review current projections and identify options to accommodate some changes in work practices to improve efficiencies.
- Track expenditures to return to normal operations and include these in the recovery plans. Investigate recovery reimbursement, grant and other programs, including federal programs. Determine your priorities (e.g., safety, operations, energy) in developing and implementing plans. Priorities may change as we become more knowledgeable about the pandemic and its impacts.
- Staffing
- Staffing plans for reopening will need to include bringing people back from furlough and how to manage COVID illness or exposure to COVID-positive individuals in quarantine/testing practice.
- Plan for employee monitoring and managing issues for illness, work from home and possible support due to school and/or child care closures.
- Compliance
- It is important to include an assessment of deferred WOs and PMs (waivers) in the recovery plan. The plan will need to include how to track progress and meet deadlines for specific waivers granted. Adjustments to plans may also be impacted by areas that are temporarily closed. Guidance from local authorities may be needed to assure compliance with regulations.
- Facility Preparation
- Facility plan for scaling operations (free units/rooms or sections of a building) should be aligned with the organization’s recovery plan, including ramping up changing or shutting down areas of the building.
- Assess and prioritize critical infrastructure restoration and reconstruction. Reevaluate the space based on the recovery plan and timetable. Perform a current status occupancy checklist that may include changes to Statement of Conditions.
- Develop strategies, implement appropriate cleaning and ready for occupancy in conjunction with infection prevention. This should include areas where COVID-positive patients were treated and COVID-positive staff worked.
- If units are closed or are being underutilized there will be a need to flush water systems on a regular basis. Consideration should also be given to treatment of the systems. Humidity and temperature logs should also be reviewed to assure that during closure or underutilization that the space was still managed to prevent mold growth.
- Perform an equipment and facility safety check. Verification of movement of equipment, etc. needs to be evaluated to assure that needed equipment is in place and ready for use.
- Create a plan and timetable to restore any building systems to pre-COVID operations, particularly mechanical systems including filters, pressurization or air handler operations.
- Review safety standard operating procedures (SOPs) for infected areas, equipment and materials. Make sure procedures are updated based upon latest COVID information.
- Check the latest CDC recommendations regarding:
- Screening patients
- Cleaning/disinfection practices
- Visitor restrictions
- Social distancing – staff and patients/visitors
- Building system guidance
- Review life safety impacts.
- Documentation
- Document lessons learned. Is there anything that should be kept in place for defined periods of time to be prepared should a second wave occur?
- What changes will need to be made to the emergency operations plans?
As the curve starts to flatten and the organization begins to look to recovery from the pandemic immediate steps will need to be taken to prepare the physical environment. This will not be an overnight return to pre-surge operations. Steps to be taken into consideration should include plans to prepare for a second surge, to reinitiate deferred services, and how and when to revert converted spaces to Non-COVID operations. Strategies need to be developed and actions taken to return spaces and systems that are critical to providing care, treatment and services in the most expeditious manner.
Immediate Needs (Days to Weeks)
- Getting Started
- Determine how to manage the recovery workload while also ramping up for deferred service. Refer to the list developed during the preplanning efforts of any services that were deferred, changes that were implemented and a variety of other considerations. Assess the staffing needs to manage the completion of the workload.
- Speak to vendors who may have discontinued coming on-site during the pandemic due to concerns for their staff to confirm they will be able to support completion of deferred activities.
- Supplement/organize workforce for response during recovery phase. Staffing plans for reopening will need to include staff to revert converted spaces and complete deferred maintenance activities. Organizations should consider using the same vendors and team members who implemented the changes to assist to revert the space. Those team members will have firsthand knowledge of how the work was completed, what changes were made and would be able to effectively revert the space. This will help take any guessing out of the equation. It is important to have a list of all the changes that were made for each space so that this can be used as a checklist with assigned tasks for the team.
- Anticipate budget impacts from reduced operations and track all expenditures. Develop a master spreadsheet of all total costs, including costs that will be associated with further demobilizing spaces that may remain for a duration in case of a supplemental surge. Include all hours worked by facilities staff including straight and overtime hours with detailed work orders. Backup documentation will be critical when applying for federal programs for reimbursement. Total project costs means all costs which have been or are estimated to be incurred including labor, materials, permits, fees for the renovation and future demobilization of spaces.
- Demobilization of Implemented Changes
- Any changes that were implemented based on surge will most likely follow the opposite progression during recovery. Determine which of the changes implemented will be reverted when. Since it is unclear if there will be future surges, determine which renovated areas will remain and how they will be used in preparation for future surges. Establishing a baseline of rooms to address potential secondary waves will be important. Understand what it took to meet the facility’s peak demand of patients on ventilators (this is crucial, at least until a vaccine is deployed).
- Planning for decreased case load and reutilization of space (reoccupancy of clinical spaces). Determine how each clinical space will be reoccupied. Reevaluate the space based on the recovery plan and timetable.
- Ramping up of “elective services” to make up financial ground may occur during this period. Across the U.S., state governors have issued orders prohibiting elective procedures. On April 19, CMS issued recommendations to reopen health care systems for the provision of elective procedures and treatment to non-COVID-19 patients. The elective and non-emergent procedure guidance relies upon states or areas passing the gating criteria before entering Phase 1 of the administration’s “guidelines for reopening America.” This requires a downward trajectory of symptoms and cases within a 14-day period and that hospitals treat all cases without crisis care and have a robust testing program in place for at-risk health care workers, including emerging antibody testing. The team will need to review what changes were made for each area that was renovated/converted. Develop a checklist with clinical operations and all departments to detail each required task. The checklist will include the task, department and owner responsible for the task and details of what needs to be completed. Some tasks cannot be performed until another task is completed, so it’s important to hold virtual meetings with all stakeholders to communicate the plan and timelines for completion.
- If units were closed or being underutilized, several steps need to be considered before occupying the unit, such as the need to flush water system on a regular basis and consider treatment of system, a facility safety check/evaluation, verification of movement of equipment, etc. Make sure humidity is reviewed during any shutdowns of areas to prevent mold growth.
- Schedule Critical Infrastructure Restoration and Repair
- Changes that may have occurred include but are not limited to modification to the HVAC system, space reconfigurations, temporary buildouts/structures, installation of negative air machines and, in some cases, modifications to duct work. Develop a complete list of modifications to document what needs to be reverted to post-COVID operations. After restoring modifications to the room pressures/duct work, you will need to test and balance the space to confirm you are meeting the requirements for air exchanges per hour (ACH) and pressure relationships.
- Review strategies and implement appropriate cleaning when ready for occupancy in conjunction with infection prevention. This should include areas where COVID-positive patients were treated and COVID-positive staff worked. Prior to restoring any areas, a terminal cleaning should be conducted by the environmental services (EVS) team. Once the terminal cleaning is complete, departments can start entering the space to demobilize. Facilities can remove any temporary barriers and HEPA machines/filters installed, convert room pressures, remove temporary differential pressure monitors, etc. Discuss with the infection prevention control (IPC) team how to handle disposal of HEPA filters, material used such as plastic barriers and items used within the space. Review safety standard operating procedures (SOPs) for infected areas, equipment and materials. Once the changes are made, EVS can conduct a final terminal cleaning.
Short Term Needs
This section addresses important issues and concerns related to the de-escalation of the event and ongoing activities. The goal is to identify needs that may continue to exist and issues that may present themselves as a result of reestablishing normal operations.
Updated guidance was issued by CMS April 19, 2020 [OPENING UP AMERICA AGAIN Centers for Medicare & Medicaid Services (CMS) Recommendations Re-opening Facilities to Provide Non-emergent Non-COVID-19 Healthcare: Phase I] for providing essential non-COVID-19 care to patients without symptoms and in regions with low and stable incidents of the virus. As part of Phase 1 in the guidelines for “Opening Up America Again,” CMS recommends that organizations plan and provide the following facility-specific items:
- Sufficient resources in order to provide care across all phases of care.
- Adequate facilities for ongoing testing and post-acute care for patients.
- Adequate facilities for operations and storage of supplies.
- Provisions for providing a healthy workforce and adequate staffing.
- Provisions for use and storage of PPE.
- Adequate resources for ongoing care, without jeopardizing potential surge capacity.
An assessment of these and other issues will be required to plan for expected and unexpected concerns during short-term operations. Example of such needs assessments include:
- Staffing and staff reorientation.
- Staff should be routinely screened for symptoms of COVID-19. If symptomatic, staff members should be tested and quarantined. Staff who will be working non-COVID care (NCC) zones should be limited to working in these areas and not rotate into COVID-19 care zones (CCZ).
- Contracted services (e.g., construction, consultation, temporary staffing).
- Workers performing these services should have knowledge of the unique intricacies of working in a hospital or other health care facility.
- These workers should be routinely screened for symptoms of COVID-19 and if symptomatic not allowed to remain on the premises.
- Workers should schedule their work such that they will be accessing either only CCZs or only NCCs on any given day.
- Workers should also be trained in the importance of not moving from a CCZ to an NCC or vice versa.
- Workers that access CCZs should be trained on how to properly access the zone, PPE required and proper decontamination procedures.
- Facility and space utilization.
- Patient care spaces require careful consideration to ensure patient and staff safety. It is important to examine changing facility needs with the assistance of qualified facilities professionals that can assess the facilities engineering controls and patient flow and help verify that response efforts will properly protect patients, staff and visitors. We strongly recommend using a multidisciplinary approach, with professionals including but not limited to:
- Facility Manager
- Infection Preventionist
- Safety/Security Manager
- Environmental Services
- Risk Manager
- Clinical Staff
- As COVID care spaces are demobilized, consider the following recommended steps to return the space to NCC patient care areas:
- Verify that all airflow relationships are correct and brought back minimally to the original design flow. If large areas are to be rebalanced, consider applying the appropriate ASHRAE/ASHE 170 standards. Ensure you have the appropriate engineering assistance to achieve this redesign.
- Verify that all pressure relationships for pressure related rooms are appropriate (e.g., soiled utility rooms are negative and clean supply rooms positive).
- Examine filtration media in air handler units to verify that mitigation efforts did not cause negative impacts and change as necessary.
- Verify that CDC recommended guidelines (see CDC Table B.1) for air changes and time required for contaminate removal based on air changes is followed.
- Verify that terminal cleaning is complete in clinical spaces and patient rooms following hospital or facility policies.
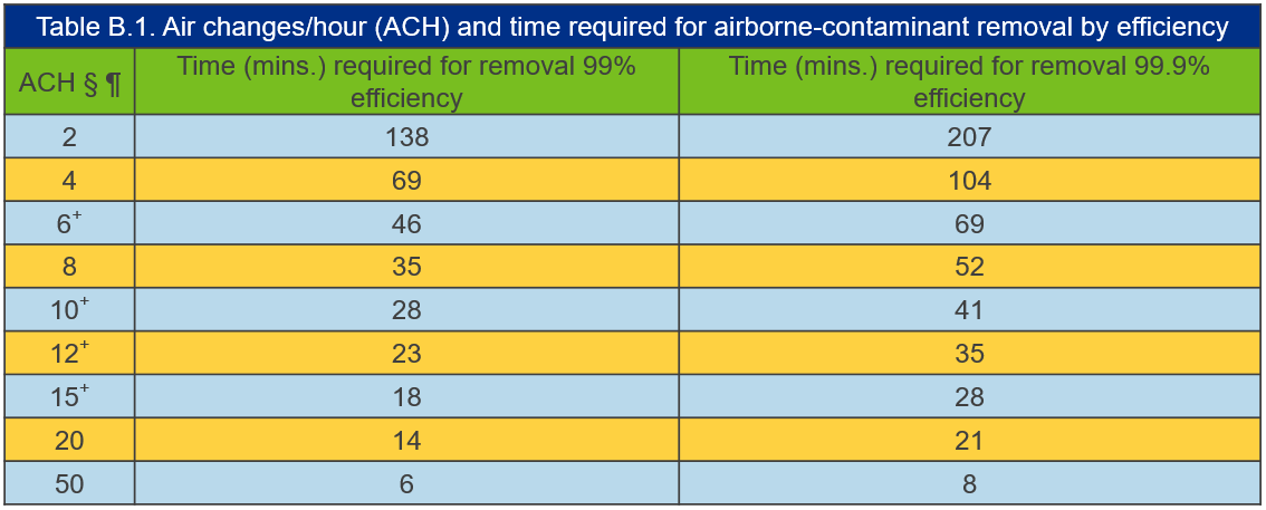
Adapted from https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html#tableb1
- Once NCC resumes, if patients are not tested prior to care (e.g., test to verify if COVID-19 positive or not the day before surgery is scheduled), the following guidance is recommended:
- Patients will be considered suspect COVID-19 patients
- Verify that CDC recommended guidelines for air changes and time required for contaminate removal based on air changes is followed after patient treatment is completed and room is vacated by the patient (see CDC Table B.1).
- Verify that terminal cleaning is completed in treatment area following hospital or facility policies.
- Patients will be considered suspect COVID-19 patients
- As non-COVID care begins to be offered the following social distancing practices should be considered:
- CMS recommends that during Phase 1, administrative and engineering controls be established to facilitate social distancing, such as minimizing time in waiting areas, spacing chairs at least six feet apart and maintaining low patient volumes. As non-COVID care begins in your facility, ASHE recommends considering the availability of hygiene products (e.g., tissues, ABHR dispensers, masks, gloves, etc.) in addition to evaluating the following social distancing practices:
- Prepare non-COVID-19 care (NCC) triage areas in order to screen non-emergent care patients as they enter the facility.
- Separate non-COVID-19 patients and COVID-19 suspect patients.
- Establish social distancing parameters within the facility such as:
- Chairs should be spaced to provide a six foot separation between itself and the next chair or seating location on all sides.
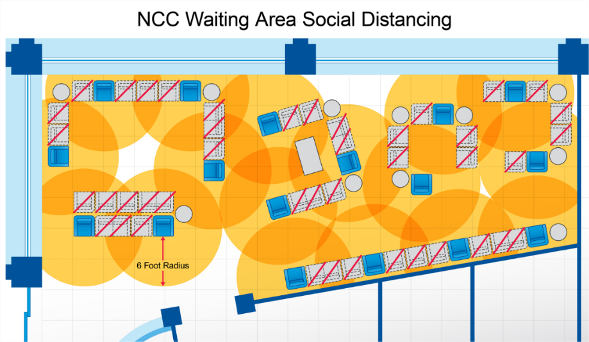
Waiting room seating that provides six foot radius around chairs.
- Markings should be provided to indicate patient spacing as shown by the red lines in the image below. Spacing should be considered in all directions (shown by yellow circles). Social distancing spacing should also be indicated where patients interact with staff, to limit staff exposure as well.
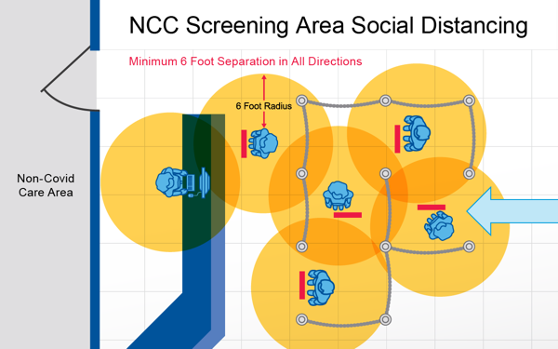
Lines indicating six foot radius spacing where queuing is expected.
- Chairs should be spaced to provide a six foot separation between itself and the next chair or seating location on all sides.
- Other assessments include:
- Additional utilities.
- Handing of patient belongings.
- Storage of additional supply.
- Provisions for monitoring needs and providing additional resources.
- Budgeting and tracking allocation of funding.
- CMS recommends that during Phase 1, administrative and engineering controls be established to facilitate social distancing, such as minimizing time in waiting areas, spacing chairs at least six feet apart and maintaining low patient volumes. As non-COVID care begins in your facility, ASHE recommends considering the availability of hygiene products (e.g., tissues, ABHR dispensers, masks, gloves, etc.) in addition to evaluating the following social distancing practices:
Decisions should be consistent with public health information and in collaboration with state public health authorities. Careful planning is required to resume in-person care of patients requiring non-COVID care.
- Patient care spaces require careful consideration to ensure patient and staff safety. It is important to examine changing facility needs with the assistance of qualified facilities professionals that can assess the facilities engineering controls and patient flow and help verify that response efforts will properly protect patients, staff and visitors. We strongly recommend using a multidisciplinary approach, with professionals including but not limited to:
Long-Term Needs
This section addresses important issues and concerns related to the long term impacts of the event and ongoing activities. The goal is to identify needs that may continue to exist and issues that may present themselves as a result of reestablishing normal operations and to apply the lessons learned from the event.
- Long-term resources
- Facilities must document the temporary changes there were made to the facility and the resources used to implement and remove these changes.
- Facilities must document the permanent changes they have made to the facility and show all appropriate documentation associated with the changes.
- Need for mass collection of data for analysis. This leads into several points below.
- Development of case studies for not only for large metropolitan areas, but for targeted rural hospitals that suffered high number of cases based on population density.
- Guide to developing strategic partnerships for sourcing supplies and materials, as well as overflow of patients, respite for staffing, etc.
- After Action Reports (AAR)
- The impacts of the pandemic will need to be documented in an AAR. Facility management needs to make sure to provide documentation of the work performed and develop corrective actions and improvement plans to address any outstanding issues.
- This AAR needs to be included as part of the emergency management program annual review.
- Corrective action plans will need to be documented as completed and included in discussions with the safety management committee to be able to be included in the minutes to close the loop for these plans.
- Need for flexibility
- Hospitals need additional rooms/suites/floors with ventilation flexibility. Not every room in the hospital needs the flexibility to switch from positive to negative, and not every room needs 12 ACH. However, best practices need to be established for existing hospitals, as well as new hospitals.
- Creating a best practices step-by-step guide for reliability centered maintenance strategies that would cut back on the burden of compliance. Many facilities personnel were tied up with converting spaces to negative pressure during the pandemic and not available to address compliance required maintenance concerns.
- Pushing for codes, CMS, AOs (including fire protection) to allow for risk assessment based ITM frequencies would have reduced the need to push ITM schedules.
- Increase the focus/push for CMS to more quickly adopt codes.
- Staffing
- Many hospitals furloughed employees, and developing a staffing plan to address the recovery efforts will be necessary. Providing a well-documented staffing plan will not only provide justification for bringing these staff members back but will also provide a timeline to do so. Unfortunately, support services were often a heavy target especially during the pandemic. Tracking of changes made and items being deferred or postponed will help to provide justification for not only staffing but also additional resources.
- This needs to include all support services staff including, facilities, security, bio-med, environmental services, landscaping, etc.
- Training plan for facilities teams to better understand how to calculate ACH and how to quickly convert rooms/areas/AHUs to negative pressure or 100% exhaust.
- For permanent 100% exhaust units/floors, facilities must understand the long-term maintenance impacts and PPE requirements. Additionally, understanding the energy impacts associated with not utilizing conditioned return air.
- Data/Best Practices
- Hospitals need data and best practices to ensure that the operational changes can quickly be made.
- Understanding of bulk oxygen and calculations to prevent freeze up.
- Understanding of how to functionally create ORs with negative pressure temporary anterooms that allow for patients to be rolled into the OR.
- Understanding of patient area HVAC system design to increase flexibility.
- Understanding of egress calculations to prevent an area from becoming too negative and preventing egress from inward swinging doors.
- Potentially look at revising how HVAs are created.
- What maintenance is essential and what can be foregone?
The New Normal
Global health care is in the midst of a modern-day, fast-paced, deadly pandemic which sadly found most countries’ health care systems greatly unprepared. Yet, as we responded using standard infection prevention practices, we have had to adjust as we better understood this novel virus that we unwittingly welcomed to our neighborhoods. Social distancing, teleworking, and hand washing have become commonplace during this time, but what, when we finally get the upper hand on our microscopic enemy, will be the new normal? And for our health care facility managers, what new baseline will we be implementing?
- What will life in health care be like after the peak, whether before or after an effective vaccine is available?
- What would a “permanent” COVID-19 unit look like?
- What new health care codes and standards might we expect?
For starters, facilities can identify/create potential surge spaces (preferably within the hospital) that can be used during normal life and quickly converted for use as COVID-19 hospital patient beds (e.g., old patient rooms being normally used for observation or exams).
The new normal may include not just having excess beds, but an entire floor or floors of truly negative pressure airborne infection isolation rooms (AIIRs) for the next wave of COVID-19 or other novel highly contagious disease. Consider equipping these rooms with vision panels in the door or corridor wall so that caregivers can visually check on the patient without donning full protective gear.
Consider making all patient rooms in the facility capable, in an emergency, of achieving a slight negative pressure.
We must rethink how we control hospital entrances. Just as the new risk for active shooters has transformed our entry/exit security, we can modify how patient traffic flows through health care facilities to prevent free access of this virus to our facilities, keeping it to limited, manageable areas.
During future waves of recurring COVID-19 (even if we have an effective vaccine), health facilities may activate their health screening protocols for all people entering the building. These would be similar to our daily go-to-work temperature checks, health questions or perhaps even requiring certificates showing evidence of vaccine or presence of antibodies. Mobile apps for these protocols are already becoming available.
For patients that have scheduled visit to the health facility there could be an electronic “pre-admission” screening on the day or day before your appointment, so you have “pre-boarding” clearance and only have to answer questions and get scanned for your temperature. This could become the new norm for all patients, not just COVID patients. Will the day come when everyone is encouraged in all seasons to not just cover their cough or wash their hands, but to wear designer cloth masks and gloves when visiting a health care facility?
There will be a need for new protocols to manage contractors working within the health facilities that may include pre-screening, daily screening, increased monitoring to ensure compliance with infection prevention practices including maintaining barriers and wearing of PPE. Criteria for preferred vendors may include requirement for all workers to have documented knowledge of the unique intricacies of working in a hospital or other health care facility along with the possibility of pre-clearances. Some contractors may have the required clearance level to work in surgical sterile corridors, or COVID-19 units, but most may not. In this way, life could go on in the midst of the COVID threat, but strictly controlled and thus helping keep the virus contained.
Materials management may enjoy a new status and be given even more space in the limited footprint of the facility to enable them to house the necessary stockpile of equipment and supplies in their arsenal to fight the corona viruses. All departments must learn how to effectively rotate supplies, so they do not expire.
There could be a need for more spaces for clinicians to practice telemedicine and corresponding spaces within long term care or other residential care facilities.
“Hardening” our Facilities for a Pandemic
How will our facility design and infrastructure be different? Facility managers and architects should come to the table to map out the new normal for health care facility design. The universal room concept has now had a chance to be tested.
Those facilities that had to come up with spur-of-the-moment COVID-19 units with negative pressure rooms may create patient care units with ventilation systems that can be easily converted from normal to negative pressure airborne infection isolation rooms or at a minimum rooms under net negative pressure.
We were fortunate this time that our COVID-19 virus chose to peak in the spring when hospitals could run their air handling systems serving the COVID-19 patient areas at 100% outside air (OA) without risk of freezing coils or not being able to keep up with heating the building. These same facilities will need to evaluate how they can achieve 100% OA in the dead of winter or investigate having HVAC units designed to be able to handle an added set of HEPA filters (to be installed during the pandemic) to simply allow return air as normal which has been HEPA filtered.
Most hospital private patient rooms of the future may have the headwall capacity (med gas, electrical outlets, etc.) to switch to semi-private rooms and accommodate twice the volume of patients.
Hospitals may plan to modify existing facilities and to construct new facilities to simplify true surge capacity (perhaps double the beds or normal census).
Plans must include the readiness of alternate care sites. While hopefully not needed, these sites will be maintained so that these facilities can be converted to functioning COVID care sites at a moment’s notice.
Permanent COVID-19 Unit
For the foreseeable future, it is hard to imagine a hospital that will not have a COVID-19 unit or at least a floor or two that could easily be converted to a COVID-19 unit. Remember when hospitals with burn units were common? The facility should identify which areas/floors of the hospital will have these units and what other health care services will be provided to COVID-19 or suspect COVID-19 patients that are located elsewhere in the hospital.
The distinct areas of the facility identified for serving COVID-positive patients can then be hardened or made in every way possible to facilitate caring for the COVID patient and controlling the spread of the virus (e.g., with ventilation, easily cleanable surfaces, closed doors, security or traffic control points, etc.)
Note: This would include asymptomatic COVID positive patients requiring heath care services (cancer treatments, emergency surgeries, urgent care, needed diagnostic services). The precautions in this document should be followed for these patients until there is a vaccine or very effective medical treatment options are available. Routine or elective treatment for COVID-19 positive patients should wait until quarantine over when patient is no longer contagious.
The Endgame
In his March 25, 2020 article in The Atlantic titled “How will the Corona Virus End?” Ed Young mentions that it is likely that the new coronavirus will be a lingering part of American life for a year or longer, but he adds: “There’s no reason that the U.S. should let SARS-CoV-2 catch it unawares again, and thus no reason that social-distancing measures need to be deployed as broadly and heavy-handedly as they now must be.
In this future, COVID-19 may become like the flu is today—a recurring scourge of winter. Perhaps it will eventually become so mundane that even though a vaccine exists, large swaths of Gen C won’t bother getting it, forgetting how dramatically their world was molded by its absence.”
Special thank you to ASHE’s COVID Recovery Team
Robert D. Booth, MPH, CIH
Senior Healthcare Consultant, Oncore, Inc.
Joshua Brackett, PE, SASHE, CHFM
Special Projects Manager, Baptist Health System
Timothy Peglow
AVP Patient Care & Prevention Facilities, MD Anderson Cancer Center
Brad Pollitt, AIA
Vice President Facilities Development, UF Health Shands
Frank D. Rudilosso, PE, M.Eng, CHSP
Director Facilities Organizational Readiness, New York-Presbyterian Hospital
Michael P. Sheerin, PE, LEED AP
Chief Executive Officer, TLC ENGINEERING SOLUTIONS®
Pier-George Zanoni, PE, CIH
Health Facilities Engineering Section, State of Michigan - Licensing & Regulatory Affairs
Disclaimer
This information is provided by ASHE as a service to its members. The information provided may not apply to a viewer’s specific situation and is not a substitute for application of the viewer’s own independent judgment or the advice of a competent professional. ASHE does not make any guarantee or warranty as to the accuracy or completeness of any information provided. ASHE and the authors disclaim liability for personal injury, property damage, or other damages of any kind, whether special, indirect, consequential, or compensatory, that may result directly or indirectly from use of or reliance on information from this webinar.